Getting consent from a patient is more than just having them sign their name on a form. Physiotherapists must ensure patients understand what they are consenting to.
This list describes what physiotherapists are required to do when obtaining consent.
The information below is a summary of the legislative requirements on consent. Refer to the legislation for full details.
- Before conducting an assessment or providing treatment, physiotherapists must get a patient’s permission to do so. This is known as consent. The physiotherapist must be sure the patient understands what is going to happen before the treatment begins by providing information about the nature of the treatment, its benefits, risks, side effects, the alternative courses of action, and any possible consequences of not having the treatment. The physiotherapist must also answer any questions the patient may ask about the treatment.
- Consent can be given verbally, in writing, or it can be implied through behaviour. For example, the patient rolls up their sleeve for their arm to be examined.
- Patients are entitled to refuse to consent to treatment or withdraw their consent at any time.
- If the patient is not capable of providing consent, the physiotherapist must find a substitute decision-maker to provide consent.
- Physiotherapists cannot make decisions on behalf of a patient. The only exception is in an emergency when there is no substitute decision-maker available to make the decisions.
- In a team environment, if there is any doubt about whether the patient provided consent to another health professional involved in the treatment plan, the physiotherapist must confirm that consent was provided or get it again.
- Physiotherapists must obtain a patient’s consent to involve others, such as physiotherapist assistants, students and volunteers, in their care. This requires a conversation with the patient about the roles and responsibilities of the physiotherapist and the physiotherapist assistant, student or volunteer.
- Physiotherapists must document their conversations with patients about ongoing consent to assessment, treatment, and involvement of other care providers, including physiotherapist assistants.
Glossary
- Capable
-
A person is capable of giving consent to treatment if they:
- Understand the information needed to make a decision concerning the treatment, and
- Appreciate the reasonably possible consequences of giving consent to the treatment or refusing to consent to the treatment.
Capacity to consent to treatment can vary over time. For example, the capacity of an elderly patient with dementia to give consent can change throughout the course of the treatment plan. The physiotherapist should therefore continuously re-evaluate the patient’s capacity.
- Substitute decision-maker
-
The substitute decision-maker is expected to make decisions based on the patient’s known wishes expressed when he or she was 16 years of age or older and capable of providing consent. The hierarchy of substitute decision-makers is:
- Guardian of the person – appointed by the court
- Someone who has been named as the person’s power of attorney for personal care
- Someone appointed as a representative by the Consent and Capacity Board
- Spouse, partner, or relative of the patient in the following order:
- Spouse or partner,
- Child, parent or a children’s aid society or other person who is lawfully entitled to give or refuse consent in place of the parent
- Parent who has only a right of access
- Brother or sister
- Any other relative (related by blood, marriage or adoption)
- Public Guardian and Trustee

Consent E-Learning Module
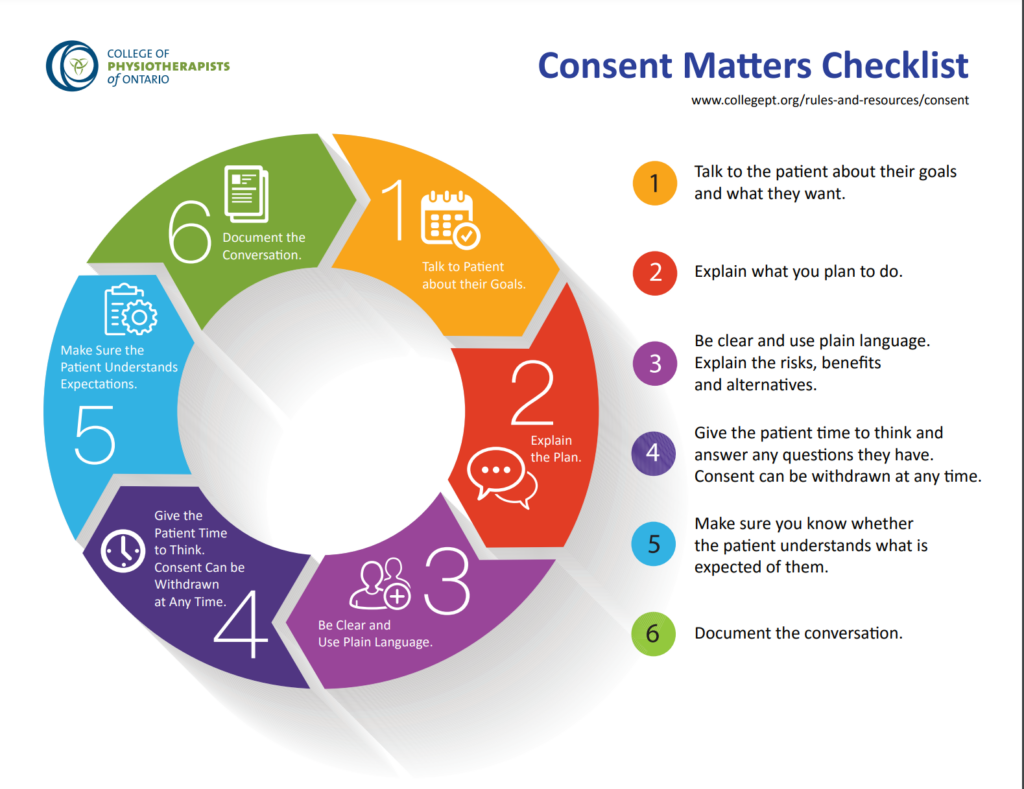
Poster: Consent Matters Checklist

Boundaries and Consent Module
From the College’s Transitioning to Practice in Ontario learning module series
Examples of Consent
It is important that physiotherapists provide written confirmation in a patient chart that the PT and the patient have had a conversation about the proposed assessment and treatment plan and all of the important elements of the consent process have been covered. Consent should always be an ongoing conversation between the patient and the health professional.
It is common for facilities to require an additional consent form be completed by the patient. This is fine, however having a patient sign a consent form is not considered getting consent. Additional written evidence that a conversation took place between the physiotherapist and the patient, and that the patient has consented to the assessment or the treatment, must be documented in the patient record.
If you have questions about how to document patient consent, please contact the College’s Practice Advice team at advice@collegept.org or 1-800-583-5885 ext. 241.
Please note: The consent samples below are only examples of different ways that a PT might capture consent in their patient records.
Consent Sample 1
Consent Sample 2
Consent Sample 3
Consent Sample 4
Learn More
CMPA Virtual Care: What About Consent?
Obtaining Consent when Custody is in Question




